Scientific background
Peri-implantitis is a pathological condition occurring in the tissue around dental implants, characterized by inflammation of the peri-implant mucosa and progressive loss of supporting bone, with no current means of cure. It affects an average of one in five patients and, due to its high prevalence, the additional cost of maintaining dental implants is five times higher than that of natural teeth. Consequently, the question of maintaining the health of dental implants and preventing peri-implantitis is a current and essential topic. The "physiological" definition of peri-implant health has evolved over time, and a diagnosis of peri-implantitis is based on a particular threshold of bone level of 3 mm below the intra-osseous part of the implant.
Thus, assessment of marginal bone level (MBL) is a major criterion of peri-implant health, and intra-oral radiographs have always been considered a reliable means of to identify defective implants. Conventional methodology for assessing this MBL is to measure bone level from a reference point such as the implant neck, shoulder, platform or abutment junction, in the direction of the bone contact, parallel to the implant axis. However, preliminary bibliographic work has shown the heterogeneity and methodological shortcomings of current proposals in this field in published published studies (absence of a gold standard for software, calibration, number of examiners, quality of radiographs used, etc.), making these bone measurements imprecise and questionable.
Internship objectives
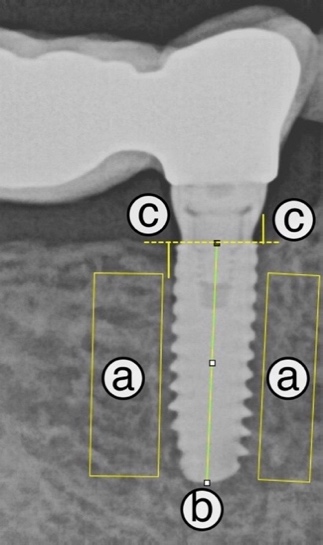 Thesis work proposed a semi-objective manual method for measuring this MBL (Figure 1). The aim is to determine:
Thesis work proposed a semi-objective manual method for measuring this MBL (Figure 1). The aim is to determine:
- (a) areas used to select the reference grey profiles of the bone on either side of the implant,
- (b-c) the dimension of the endosseous part of the implant used for radiographic scaling,
- (c) tracings to assess the marginal bone level on the mesial and distal sides from the implant neck (dotted lines c-c).
The areas (a) are then used to manually determine where the bone ends on either side of the implant neck.
Note that 124 implants from two sets of X-rays, corresponding to 496 measurements, have already been annotated.
The aim of this internship is to propose an automatic or semi-automatic method for making this measurement, free from the subjectivity of the annotator.
This work involves several stages:
- understanding the medical context and data,
- proposing a method for finding the implant axis and neck,
- proposing a method for determining the areas where bone is present,
- propose a method for estimating peri-implant marginal bone level (MBL),
- test and evaluate these methods,
- develop a graphic interface for dentists.
Skills required
- Signal and Image processing
- Statistics and Machine Learning
- Python programming
- Interest in medical imaging in general, and dental radiography in particular
Informations
- Duration of internship: 6 months
- Location: Laboratoire Créatis, Laboratoire Multimatériaux et Interfaces et faculté d’odontologie, Lyon
- Supervisors: Doriane Chacun, Fabien Millioz
- Send CV, covering letter and latest transcript to doriane.chacun@univ-lyon1.fr and fabien.millioz@univ-lyon1.fr
References
- [1] J. Derks and C. Tomasi. Peri-implant health and disease. a systematic review of current epidemiology. Journal of Clinical Periodontology, 42(S16):S158–S171, 2015.
- [2] D. Herrera et al. Prevention and treatment of peri-implant diseases-the EFP S3 level clinical practice guideline. J. Clin. Periodontol., 50 Suppl 26(S26):4–76, June 2023.
- [3] T. Berglundh et al. Peri-implant diseases and conditions: Consensus report of workgroup 4 of the 2017 world workshop on the classification of periodontal and Peri-Implant diseases and conditions. J. Clin. Periodontol., 45 Suppl 20:S286–S291, June 2018.
- [4] K. Gröndahl and U. Lekholm. The predictive value of radiographic diagnosis of implant instability. The International journal of oral & maxillofacial implants, 12 1:59–64, 1997.
- [5] H. P. Weber et al. Radiographic evaluation of crestal bone levels adjacent to nonsubmerged titanium implants. Clinical Oral Implants Research, 3(4):181–188, 1992.
- [6] D. Chacun. Critères de jugement en implantologie orale : intérêts et limites d’investigation de la bio-intégration implantaire in vivo. PhD thesis, École doctorale Interdisciplinaire Sciences-Santé, 2022.
